A Softball Coach's Guide To Managing Pitching Injuries
A Softball Coach's Guide To Managing Pitching Injuries
Up to two-thirds of NCAA Collegiate pitchers report shoulder or arm pain at some point in the season. Dr. Kaila Holtz offers a guide to preventing injuries.

Dr. Kaila Holtz is a Sports Medicine Physician with expertise in softball and baseball injuries based in Vancouver, British Columbia. She competed for Canada in the 2004 Olympics and has coached youth pitchers for over 15 years. In addition to clinical practice she is the Chief Medical Officer for Plantiga, a wearable insole sensor company. She is a scheduled speaker at PitchStock hosted by S2Breakthrough, July 2020 in Chicago, IL. Twitter: @KailaHoltz
Throwing related injuries are inevitable, even at the highest level of competition. Up to two-thirds of NCAA Collegiate pitchers report shoulder or arm pain at some point in the season. After a weekend of travel ball, pitchers ages 14 to 18 years report pain and fatigue without full recovery in between competition days. Shoulder injuries affect the game performance of roughly one-third of youth softball pitchers over the course of a season. The myth that softball pitching is “safer” than baseball pitching has been debunked by biomechanists so let’s just all agree; arms will hurt if you wind them in a circle over, and over, again.
As a Sports Medicine Physician who treats both softball and baseball athletes I suggest coaches take the following approach to pitching related pain this year.
1) Screen your pitchers for shoulder and arm complaints.

Assume on a team with three starters that at least one pitcher will be throwing with pain that limits their performance. Knowing who is more likely to have pain before the season even starts would be helpful in managing workloads and rest days.
I suggest using the Kerlan-Jobe Orthopedic Clinic Questionnaire (KJOC). In 2018, we published a small study showing that youth softball pitchers with a pre-season KJOC score less than 90 had a higher risk of in-season injury. The same cut-off scores have been suggested in professional baseball to detect healthy vs. at-risk arms. The questionnaire takes 10-15 mins for teams to complete.
2. Have someone with experience in athlete assessments examine your athletes who are at the highest risk for an in-season injury.

“Movement Screens” are ubiquitous in youth and professional sports right now. I think they’re great because they can identify strengths and weaknesses in an athlete’s movement pattern but there are some drawbacks to be aware of:
- Many are validated in adult male populations (e.g. military, fire or police)
- Conflicting evidence whether they predict injuries or performance.
Look for an individual or company with functional anatomy training, experience with athletes across a spectrum of developmental stages and a sound understanding of throwing/pitching biomechanics. A weekend or online certification shows interest in the topic but not necessarily expertise.
3. Get some baseline data.
It’s exciting to see analytics in baseball and softball spilling over to sports medicine, a field called injury analytics. As part of an athlete assessment or pre-season training camp the most valuable tests in predicting in-season throwing injuries are:
- Passive total range of motion of the shoulder (TROM)
- Single-leg tests
- Countermovement and cyclic jumps
Total range of motion is tested with the athlete laying on their back (supine) on a bench or examining table. Passive external rotation and internal rotation are measured using a goniometer and added for a total range of motion measures. Studies in baseball pitchers suggest a TROM difference of greater than 5° (non-dominant vs. dominant arm) to be a risk factor for elbow injuries. I use TROM as a screen for muscle imbalances like a tight latissimus dorsi or pectoralis muscles in my softball athletes.
The Y Balance test is a relatively inexpensive way to screen single-leg functional strength and lumbopelvic control. The test requires the athlete to stand on one leg and move a measuring tool in the anterior, posterolateral and posteromedial directions with the other foot. Y Balance test score is calculated by adding the sum of the three reach directions, dividing by the leg length and then multiplying by 100.
Here are some Y Balance Test norms for NCAA Div I female athletes:
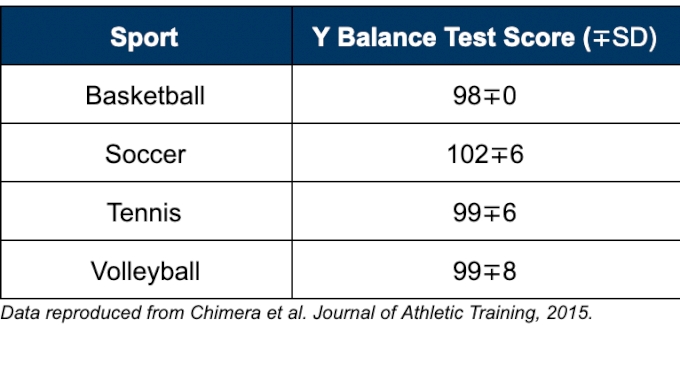
There are Y Balance test norms for male baseball pitchers with ulnar collateral ligament injuries vs. healthy controls but no one yet has published beyond static measures of hip internal and external rotation in female softball pitchers.
Lastly, jump tests have largely replaced static movement screens for talent identification and injury risk prediction in high-performance sport for several reasons: they’re objective, they correlate to on-field performance, they are sensitive to fatigue and results can be easily tracked over time.
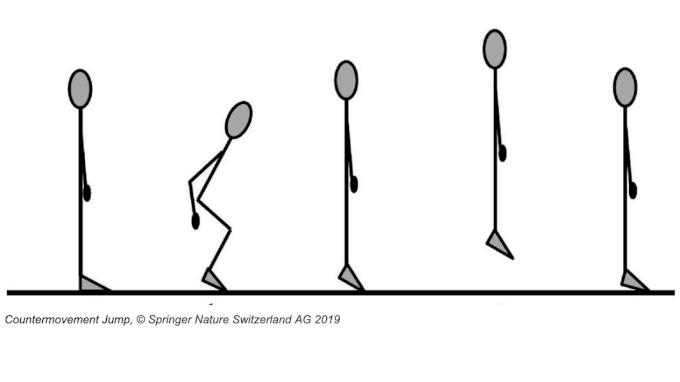
Jump tests including the countermovement jump, one leg hop and cyclic jump tests have been correlated with injury risk in adolescent females (e.g. anterior cruciate ligament rupture) and can be used track neuromuscular fatigue over the course of a season. Jump tests are usually performed on portable force plate or pressure sensor in a laboratory setting but with machine learning companies like Plantiga are bringing lab grade jump/run/walk and workload data to clinicians and coaches on the field using insole sensors that fit in your cleats.
4. Understand how the kinetic chain works and how to apply it to pitching.
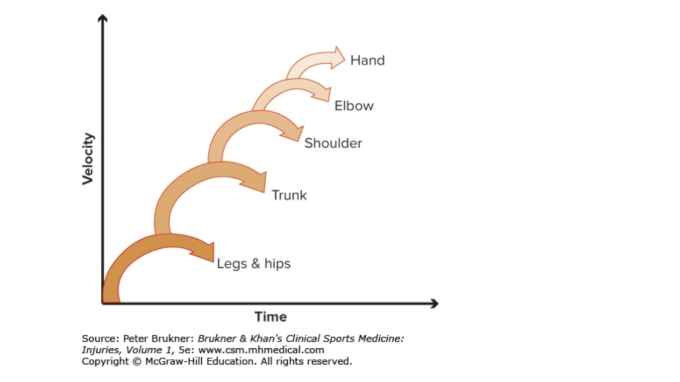
“The kinetic chain is a term for sequential activation, mobilization, and stabilization of body segments to generate and regulate force to produce motion and protect tissues from increased strain during an athletic activity”
- Dr. Ben Kibler, Orthopedic Surgeon and Kinetic Chain Guru
I love this definition of the kinetic chain by Dr. Ben Kibler who takes a very nuts and bolts approach to force transfer. He describes a stable pelvis and scapula as a means to be able to funnel forces through the relatively unstable glenohumeral joint at the shoulder to the arm out the wrist and hand.
To create a stable pelvis and scapula in softball pitching two things have to happen. First, the arm needs to be at roughly 150 degrees of shoulder abduction at landing, and second, medial rotation of the back thigh needs to start prior to pelvic rotation which starts prior to upper body rotation. In fact medial rotation of the back thigh in pitching (like throwing) should probably start even before the front foot touches down.

It is critical coaches understand these principles because incorrect sequencing results in anterior shear forces at the shoulder causing biceps tendon and rotator cuff pain. If the back thigh extends rather than rotates the pitcher usually lands early and the kinetic chain potential is cut in half. Pitchers landing early are forced to rotate their shoulders toward the catcher to push the ball to its release point with muscle energy rather than centripetal force. Commonly this is seen as the glove side “swimming” in an effort to create rotation when it’s not coming from the ground up. Many strong athletes can get away with throwing this way but inevitably their arm will be sore and pitch velocities will top out in the high 50’s, low 60’s.
Two common reasons for kinetic chain sequencing errors in youth softball pitchers are: weakness in lumbopelvic and scapular control and improper cueing. I routinely ask athletes with arm injuries on how often they perform one-leg balance or plank based strengthening activities as part of their training. Overwhelmingly this is, “almost never”. Even with the proper cues if athletes have weak gluteal and deep core muscles they will not be able to balance on their back leg long enough to medially rotate it properly prior to landing.
There are several fantastic online resources on functional strength training for throwing athletes (i.e Austin Wasserman and HLT) and I highly consider adding exercises like side plank, front plank with leg lifts, split squat and speed skater jumps to your team’s warm-up routine. I would even consider transferring the bands misguidedly used for upper body “activation” to the lower body and do lateral band walks for gluteus medius strengthening instead.

When it comes to technical cueing errors I would offer that every coach has their implicit bias when it comes to describing and teaching pitching mechanics. Some of us focus on start sequencing and leg drive while others hone in on arm position at landing or degree of pelvic rotation at ball release. Very few of us are talking about the sequence of the kinetic chain.
As I spoke about at PitchStock last July in Chicago, we’ve known the proper kinetic chain sequencing in softball pitching since 1998. Steven Barrentine a student in Dr. James Andrew’s biomechanics laboratory described that maximum pelvis rotation occurred prior to maximum upper torso rotation (i.e. the hip-shoulder separation described in baseball pitching and hitting) but amongst coaches this knowledge has been slow to trickle down.

Example of hip-shoulder separation in softball pitching by Yukiko Ueno of Japan.
We’ve been distracted by our observations of static photo images until recently as smartphone video capture technology has improved to the point where we can have video analysis apps like Coaches Eye with us at practice. It’s exciting to see several softball focused biomechanics laboratories and companies like S2Breakthrough emerging which I believe will only serve to enhance our understanding of the kinetic chain in softball pitching further.
Lastly, one cannot forget that our athletes are human beings with nervous systems overlaying the thigh, torso and arm segments measured with biomechanics markers. Neuromuscular activation cues are an emerging area of sports performance coaching and certainly something worth exploring further as a technical coach. Especially if you have hypermobile athletes that struggle to control their core position during complex movements. I call neuromuscular cues the “magic sauce”.
5. Have a responsive team to support athletes.
Because arm injuries are bound to occur as a natural consequence of pitching at a high level, I strongly recommend all athletes have a family physician or primary care provider. These individuals will be able to access imaging or refer on to Physical Therapy or Sports Medicine/Physiatry/Orthopedic Surgery when red flags are present.

I also recommend athletes with a history of upper extremity or back injuries to establish a relationship with a local Physical Therapist, Sport Chiropractor, Certified Massage Therapist or Athletic Trainer. Preferably this is an individual that has some expertise in throwing related injuries and can help guide athletes through transient arm soreness and activate when it might be appropriate to see a Physician for assessment.
Summary
Anticipating that your throwing athletes will struggle with shoulder or arm pain at some point in the season ensures a proactive rather than reactive response when it happens. Involve athletes in understanding how they can create and funnel force from their lower to their upper body and give them a clear pathway to seek help if they are underperforming because their arm is sore. Lastly, consider collecting meaningful data to track athletes before and during the season. Informed decision making is key to minimize our internal biases and allows us to evaluate our own practices when it comes to the injury prevention and management of our athletes.
References available upon request.
If you wish to chat further or need help finding an appropriate health care professional in your area schedule a phone call or video meeting on PickMyBrain here: https://www.pickmybrain.world/profiles/kaila-holtz/
References:
Hill JL, Humphries B, Weidnier T, Newton RU. FEMALE COLLEGIATE WINDMILL PITCHERS: INFLUENCES TO INJURY INCIDENCE. J Strength Cond Res 2004; 18: 426–431.
Skillington, S. A., Brophy, R. H., Wright, R. W., & Smith, M. V. (2017). Effect of Pitching Consecutive Days in Youth Fast-Pitch Softball Tournaments on Objective Shoulder Strength and Subjective Shoulder Symptoms. The American Journal of Sports Medicine, 45(6), 1413–1419.
Holtz, K. A., & O’Connor, R. J. (2018). Upper Extremity Functional Status of Female Youth Softball Pitchers Using the Kerlan-Jobe Orthopaedic Clinic Questionnaire. Orthopaedic Journal of Sports Medicine. Open access online.
Barrentine, S., Fleisig, G., Whiteside, J., Escamilla, R., and Andrews, J. (1998). Biomechanics of Windmill Softball Pitching With Implications About Injury Mechanisms at the Shoulder and Elbow. Journal of Orthopaedic & Sports Physical Therapy 1998 28:6, 405-414
Rojas, I. L., Provencher, M. T., Bhatia, S., Foucher, K. C., Bach, B. R., Romeo, A. A., … Verma, N. N. (2009). Biceps Activity during Windmill Softball Pitching: Injury Implications and Comparison with Overhand Throwing. The American Journal of Sports Medicine, 37(3), 558–565.
Bonazza, N. A., Smuin, D., Onks, C. A., Silvis, M. L., & Dhawan, A. (2017). Reliability, Validity, and Injury Predictive Value of the Functional Movement Screen: A Systematic Review and Meta-analysis. The American Journal of Sports Medicine, 45(3), 725–732.
Moran RW, Schneiders AG, Mason J, et alDo Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysisBritish Journal of Sports Medicine 2017;51:1661-1669.
Chimera, N. J., Smith, C. A., & Warren, M. (2015). Injury history, sex, and performance on the functional movement screen and Y balance test. Journal of athletic training, 50(5), 475–485. https://doi.org/10.4085/1062-6050-49.6.02
Naomi Datson, Matthew Weston, Barry Drust, Warren Gregson & Lorenzo Lolli (2019) High-intensity endurance capacity assessment as a tool for talent identification in elite youth female soccer, Journal of Sports Sciences,DOI: 10.1080/02640414.2019.1656323
Gustafsson, J. (2019). Rebound jump test to measure neuromuscular fatigue : An attempt to understand training readiness and minimize injury incidence in youth team sports (Dissertation). Retrieved from http://urn.kb.se/resolve?urn=urn:nbn:se:lnu:diva-80706
Putnam CA. Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech 1993; 26: 125-135.